 Antibiotics
Antibiotics
Drugs and Superbugs
Since the discovery of Penicillin, nearly 100 years ago, antibiotics have been used in medicine and allied industries in the fight against disease causing bacteria. Sadly due to our excessive and uncontrolled use of these substances, bacteria have begun to resist antibiotics, the dawn of the “superbug”.
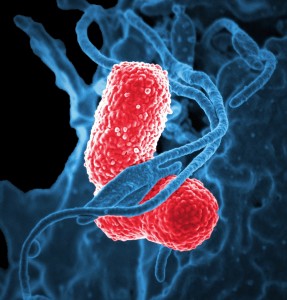
Superbug is a term used to describe bacterial strains that have developed an immunity to multiple antibiotics that can no longer kill them [1]. Some of these superbugs include multi-drug- resistant tuberculosis (not transmitted through food) and an emerging food pathogen Klebsiella pneumonia, a major cause of pneumonia.
Although not commonly categorised as a food borne pathogen, Klebsiella pneumonia has emerged as a contaminant in a number of studies in the US on retail meat and poultry. These respective studies showed that 14% of Chicken samples and 47% of meat samples tested contained the pathogen. Even more alarming is that 8.5% of the Klebsiella pneumonia were multi- drug resistant. These studies also showed startlingly high levels of drug resistance among Salmonella (38%) and E.coli (40%) isolated from these meat samples [2].
In South Africa numerous studies have been done on bacteria isolated from cattle and poultry that have shown many of these to be resistant to at least one antibiotic. Notably, resistance to Avoparcin, which has been banned since the early 90s was found in 66% of E.coli isolates from poultry in a study conducted in 2002. Avoparcin was banned internationally due to its close relations to Vancomycin, a last line of defence against multiple drug resistant bacteria [3].
The regulations governing the maximum limits for veterinary medicine and stock remedy remedy residues (R. 1809 of 1992) governs the use of antibiotics in livestock in South Africa. These regulations have been written with the intension of regulating the maximum allowable levels in food consumed by the consumer and are not aimed at controlling the use and abuse of antibiotics by the producer. Apart from treating disease, it has been common practice in South Africa to use antibiotics as a prevention against disease and as growth promoters [3].
Studies have shown that over time bacteria are able to build up a tolerance to these low levels of antibiotic, acquiring and transferring these resistance genes amongst each other. The cattle and their manure become major vehicles for transferring these resistant bacterial strains to farm personnel [4]. Further human-to-human contact spreads the bacteria and their resistance genes along with them. In other cases the cattle are slaughtered and the resistant bacteria are passed onto the consumer via the meat.
In light of this, although regulations are in place to control maximum residue limits of antibiotics in meat and poultry, it is the responsibility of the producer to be due diligent. Farmers would do well to consider the implications of using antibiotics, except for the treatment of disease.
Article by: David James Scott
References:
1. National Institutes of Health, News in Health 2014. Stop the spread of Superbugs: Help fight drug-resistant bacteria. Available from:<https://newsinhealth.nih.gov/issue/ feb2014/feature1>. [12 Feb 2016].
2. Consumer Reports, Product Reviews 2014. Dangerous contaminated chicken. Available from: <http:// www.consumerreports.org/cro/magazine/2014/02/the-high- cost-of-cheap-chicken/index.htm>. [12 Feb 2016].
3. Henton, M.M. Eagar, H.A. Swan, G.E. van Vuuren, M. 2011. Part VI. Antibiotic management and resistance in livestock production. SAMJ 101(8).
4. Bester, L.A. Essack, S.Y. 2010. Antibiotic resistance via the food chain: fact or fiction? South African Journal of Science 106(9/10) Art. 281.